New scientific findings suggest that menopause may be linked to brain changes similar to those seen in the early stages of Alzheimer’s disease, offering fresh insight into why women face a higher risk of developing dementia later in life.
The research adds to a growing body of evidence that hormonal changes during menopause may play a critical role in brain aging, long before memory problems or cognitive symptoms become noticeable.
What the Research Found
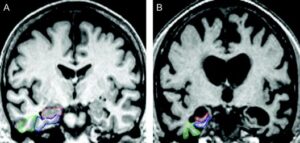
Scientists observed that women transitioning through menopause showed measurable changes in brain structure, metabolism, and energy use. These changes closely resemble patterns commonly associated with early Alzheimer’s disease — even in women who showed no outward signs of cognitive decline.
Key observations included:
-
Reduced brain glucose metabolism
-
Subtle structural brain changes
-
Alterations in neural connectivity
-
Early markers linked to memory and learning regions
Researchers stress that these findings do not mean menopause causes Alzheimer’s, but rather that menopause may represent a biological window of vulnerability for brain health.
Why Menopause Affects the Brain

Menopause is marked by a sharp decline in estrogen — a hormone known to support:
-
Brain energy production
-
Synaptic health
-
Neural communication
-
Protection against inflammation
As estrogen levels fall, the brain may be forced to adapt its energy systems, potentially triggering changes that resemble those seen in neurodegenerative conditions.
This may help explain why nearly two-thirds of Alzheimer’s patients are women.
Early Changes, Not a Diagnosis
Experts emphasize that the observed brain changes:
-
Occur years or decades before Alzheimer’s symptoms
-
Do not guarantee future dementia
-
May be reversible or adaptable
In many cases, the brain appears to reorganize and compensate, suggesting menopause may be a transition period rather than a point of permanent decline.
Why This Matters for Women’s Health
Historically, Alzheimer’s research has focused heavily on aging, with less attention to sex-specific biological factors. These findings highlight menopause as a crucial — and previously under-recognized — stage in women’s neurological health.
Understanding these changes could:
-
Improve early risk assessment
-
Shape personalized prevention strategies
-
Influence decisions around hormone therapy
-
Encourage earlier cognitive health monitoring
Potential Implications for Prevention
While no single intervention can prevent Alzheimer’s, researchers suggest that midlife may be a key opportunity for protective action, including:
-
Managing cardiovascular health
-
Maintaining physical activity
-
Supporting metabolic and brain health
-
Addressing sleep and stress
-
Monitoring cognitive changes proactively
Future research may clarify whether targeted treatments during menopause could reduce long-term dementia risk.
A Shift in Alzheimer’s Research
The findings signal a broader shift in how scientists approach Alzheimer’s disease — moving away from viewing it solely as a disease of old age, and toward understanding it as a long, gradual process influenced by midlife biology.
Menopause, researchers say, may be one of the earliest detectable turning points in that process for women.
Final Take
The link between menopause and Alzheimer’s-like brain changes underscores the importance of early brain health awareness for women. Rather than being a cause for alarm, the research offers an opportunity — to identify risk earlier, personalize care, and rethink how women’s cognitive health is supported across the lifespan.
As science continues to uncover how the female brain ages, menopause is emerging not just as a reproductive milestone, but as a critical chapter in long-term neurological health.



